The following is a guest blog post by Shahriar Shakeri, MD, MPH using analysis from the Massachusetts Healthy Aging Data Reports:
Cardiovascular disease (CVD) remains one of the leading causes of death among older adults in the United States. However, the burden of cardiovascular disease is not experienced equally across different communities in Boston. This study examines how socioeconomic conditions, environmental factors, and access to care shape cardiovascular outcomes among adults aged 65 and older.
By comparing Back Bay and Beacon Hill (higher-income neighborhoods) with Roxbury and Mission Hill (lower-income neighborhoods), this study highlights how deeply social determinants of health and structural inequities affect healthy aging across the city.
Data were obtained from the 2025 Massachusetts Healthy Aging Data Report (Dugan, E., Lee, C.M., Jansen, T., Song, Q., Su, Y.J., & Silverstein, N.M. The Massachusetts Healthy Aging Data Report: 2025 Highlights. (https://mahealthyagingcollaborative.org/data-report/explore-the-profiles/).
Key Findings
- Older adults in Roxbury and Mission Hill experience significantly higher rates of cardiovascular disease and related chronic conditions
- Emergency room visits and hospitalizations are nearly twice as high in lower-income neighborhoods
- Cardiovascular risk factors, including smoking, physical inactivity, obesity, and diabetes, are more prevalent in lower-income neighborhoods
- Food insecurity, economic instability, limited spaces for physical activity, and digital access gaps remain major barriers
- Preventive care access and service utilization remain uneven despite high rates of having a regular healthcare provider
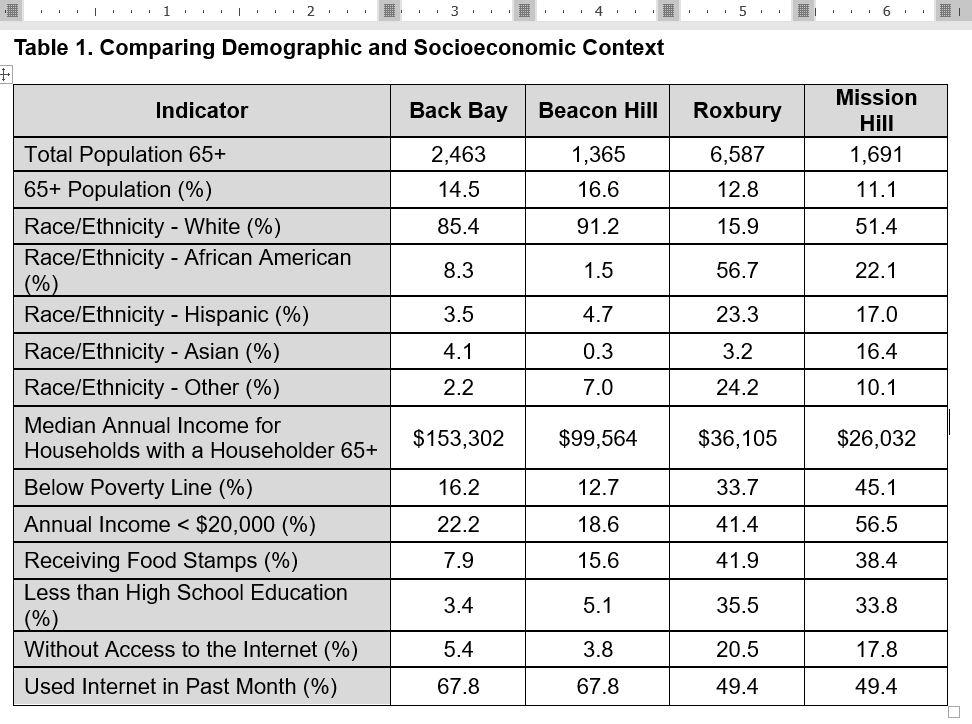
Demographic and Socioeconomic Conditions
Significant socioeconomic inequities exist between the selected neighborhoods. Older adults living in Roxbury and Mission Hill experience:
- Markedly lower median household incomes
- Higher poverty rates
- Greater reliance on food assistance
- Lower educational attainment
- Lower access to and use of the internet
These conditions directly influence access to healthcare services, preventive resources, nutrition, and opportunities for physical activity.
Black and Hispanic populations experience a disproportionate burden of cardiovascular disease compared with White individuals. A higher proportion of Black and Hispanic older adults reside in Roxbury and Mission Hill than in Back Bay and Beacon Hill, which contributes to observed disparities in cardiovascular health outcomes.
Table 1. Comparing Demographic and Socioeconomic Context
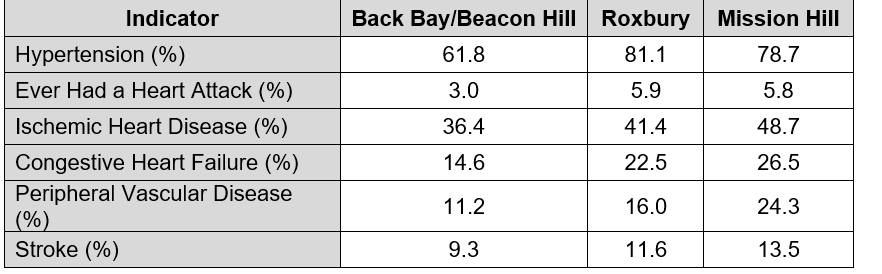
Cardiovascular Disease Outcomes
Cardiovascular disease burden is disproportionately higher among adults aged 65 and older living in Roxbury and Mission Hill. Compared with Back Bay and Beacon Hill, these neighborhoods demonstrate:
- Higher prevalence of hypertension
- Higher rates of heart attacks and ischemic heart disease
- Higher rates of congestive heart failure
- Higher rates of peripheral vascular disease and stroke
These patterns reflect the cumulative impact of economic stress, environmental exposure, limited access to preventive care, and long-standing structural inequities.
Table 2. Cardiovascular Disease Outcomes
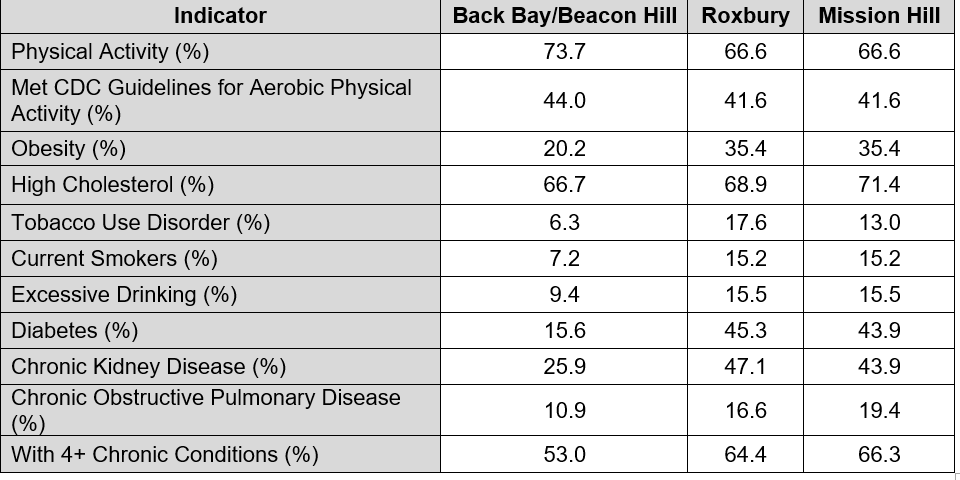
Cardiovascular Risk Factors
Cardiovascular risk factors are also significantly higher among older adults in lower-income neighborhoods:
- Higher obesity prevalence
- Nearly three times the rate of diabetes
- Substantially higher rates of tobacco use
- Greater prevalence of excessive alcohol consumption
- Lower levels of physical activity
- Higher rates of multi-morbidity (four or more chronic conditions)
Table 3. Related Risk Factors
Healthcare Access and Utilization
While most adults aged 65 or older across all neighborhoods report having a regular healthcare provider, important differences exist in how care is utilized:
- Emergency room visits are dramatically higher in Roxbury and Mission Hill
- Inpatient hospitalizations occur at nearly double the rate
- Dual Medicare–Medicaid eligibility is far more common
- Routine physician visits are fewer per year
These patterns suggest barriers to timely preventive and outpatient care, potentially leading to increased reliance on emergency services.
Table 4. Healthcare Access and Service Utilization

Public Health Implications
Advancing healthy and equitable aging in Massachusetts requires coordinated, multi-sector solutions. These findings support the need to:
- Expand community-based chronic disease prevention and management programs
- Improve access to and utilization of preventive screenings and medications
- Invest in safe, accessible spaces for physical activity, such as walking spaces and green areas
- Enhance healthy food access and nutrition support systems
- Expand digital access for older adults
- Deliver culturally responsive and linguistically appropriate care
Conclusion
This neighborhood-level study demonstrates that cardiovascular health is deeply related to social and structural conditions. The findings suggest that older adults in Roxbury and Mission Hill experience significantly higher burden of cardiovascular disease due to longstanding inequities in income, food access, healthcare access and utilization, built environment, and education.
Addressing cardiovascular disparities in Boston will require sustained policy action, cross-sector collaboration, and community-driven solutions that reflect the lived realities of aging residents. Clinical care alone is not sufficient; improving the environments in which people live, work, and age is essential to achieving health equity.
The Massachusetts Healthy Aging Collaborative remains committed to supporting communities in becoming more age- and dementia friendly with actionable data, partnership and funding opportunities, and advocacy to ensure that every older adult has the opportunity to age with health, dignity, and equity.
